Laser therapy Light energy

How does laser therapy work?
Therapeutic effects
High power and low power.
Emission mode.
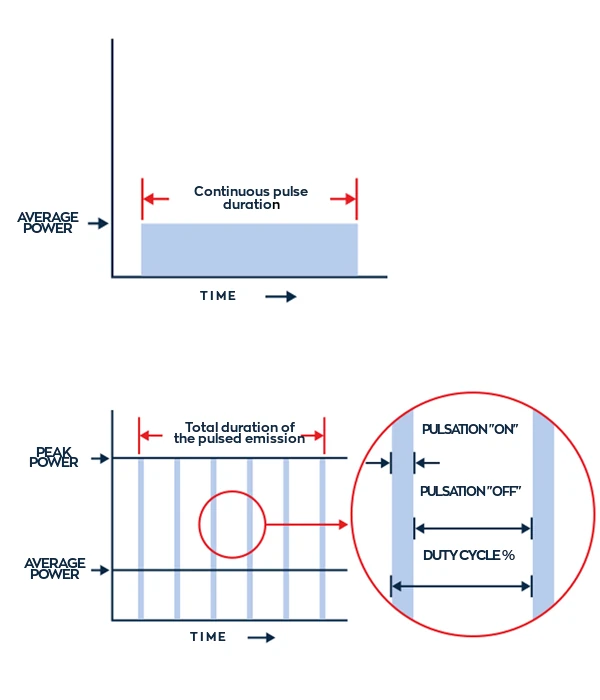
Another parameter to consider, depending on the therapeutic objective, is the type of emission. Incontinuous emission, the laser produces constant power when active.
With continuous emission, the beam is emitted without intermittence: the frequency will be = 0, so the average and peak power of the laser beam will be equal.
In pulsed mode the emission takes place at higher or lower frequencies that allow the emission of short-lasting, high-intensity pulses. In this mode there is an average power and a peak power.
Part of the pulsed mode is the Duty Cycle: with the Duty Cycle it is possible to deliver high energy doses to the body, but without overheating (and thus damaging) the tissue.
Wavelength
GLOBUS laser devices allow for the use of three different wavelengths, which fit into the so-called 'therapeutic window', i.e. the range in which absorption by the passive chromophores of the human body is most limited.
Clinical laser therapy studies
Low-level laser therapy (LLLT) is believed to have an analgesic and biomodulatory effect on microcirculation.
This study was designed to examine the pain-relieving effect of LLLT and potential changes in microcirculation measured by thermography in patients with knee osteoarthritis (KOA).
Patients with mild to moderate KOA were randomly divided into groups to receive LLLT or placebo LLLT. Treatments were delivered twice a week for a period of 4 weeks with a diode laser (830 nm wavelength, continuous wave, power at 50 mW) in skin contact at a dose of 6 J/point.
The placebo control group was treated with an ineffective probe (power 0.5 mW) of the same aspect. An evaluation with thermography (bilateral comparative thermography with AGA infrared camera) was performed prior to treatment, then once a week during the course of treatment and then two weeks and two months after completion of the sessions.
Joint flexion, circumference and pressure sensitivity were measured; the visual analogue scale was also recorded. In the group treated with active LLLT, significant improvement was found in pain (before treatment: 5.75; 2 months after treatment: 1.18); circumference (before treatment: 40.45; after treatment: 39.86); pressure sensitivity (before treatment: 2.33; after treatment: 0.77); and flexion (before treatment: 105.83; after treatment: 122.94). In the placebo group, changes in joint flexion and pain were not significant.
Thermographic measurements showed an increase in temperature of at least 0.58°C and thus an improvement in circulation compared to initial values.
In the placebo group, these changes did not occur. Our results show that LLLT reduces pain in KOA and improves microcirculation in the irradiated area.
Chronic pain of the foot and ankle joints is one of the most common complaints in our medical establishment.
In previous studies, benefits of low level laser therapy (LLLT) have been reported for chronic pain in the elbow, hand, fingers and lower back.
This study examined the effects of LLLT on chronic pain in the foot and ankle joints.
In this study, 17 subjects with chronic foot or ankle pain (of different nature) received therapy with LLLT (1000 mW, 20J/cm², 830 nm, continuous emission).
Each subject received two treatments per week for 4 weeks. A visual analogue scale (VAS) was used to report the effects of LLLT therapy on chronic pain, and a significant improvement in symptoms was noted at the end of the treatment cycle.
All but two patients showed an improvement in symptoms: excellent (2) and good (13). After treatment, however, no significant differences were observed in the range of motion of the ankle joint.
Discussions with patients also addressed the importance of good walking posture and how not to overload the ankle joint.
This study showed that LLLT was an effective form of treatment for chronic foot and ankle joint pain in combination with postural education during all daily activities.
The temporomandibular disorder is a generic term used to group all clinical signs and symptoms involving the masticatory muscles, the temporomandibular joint (TMJ) and associated structures.
As temporomandibular disorder is multifactorial, there are several therapeutic modalities to eliminate signs and symptoms.
LLLT (low level laser therapy) is commonly used for pain reduction and acceleration of healing processes.
The aim of this study was to evaluate the effectiveness of LLLT at 980 nm on patients with temporomandibular disorders.
A total of 48 subjects with (non-degenerative) temporomandibular disorders were randomly divided into two groups.
In the study group, patients underwent LLLT (980 nm, 80 Hz, 6 J) on three points of the temporomandibular joint for one minute. In the placebo group, the laser device was positioned and set with the same parameters but without emission.
Re-evaluation of pain and temporomandibular clicking was done after 2 days, after 4 days, after 6 and after 12 months. Pain intensity after 4 days in the study group was significantly lower than in the placebo group (2.4±1.36 VS 4.4±1.84). The reduction in temporomandibular click was 23.1% in the placebo group and 76.3% in the study group.
The results were statistically significant for both pain and clicking up to 2 years of follow-up with no recurrences.
LLLT at 980 nm is therefore effective in the management of temporomandibular disorder in terms of reducing pain and clicking in patients with non-degenerative TMJ disorders.
Bariatric surgeries are effective techniques for weight loss in cases of obesity: however, it remains an invasive procedure and post-surgical complications can occur.
LLLT (low level laser therapy) is increasingly used for its efficacy in controlling the inflammatory response, accelerating tissue repair and reducing pain.
The aim of this study was to investigate the effects of photobiomodulation after bariatric surgery and to understand the mechanisms of laser action on the inflammatory process, wound healing and pain.
Eighty-five gastric bypass surgery subjects were divided into two groups and underwent LLLT therapy at 10 different sites of the surgical scar.
The study group (43 patients) received active laser therapy while the placebo group (42 patients) was treated in the same way but with the device switched off.
The device used for the therapy (and which was used above the abdominal wound, approximately 1 cm from its perimeter) was a diode laser, with a wavelength of 808 nm, used in continuous emission mode, fluence 10J/cm², power 100 mW, time 20 seconds per spot, spot area 0.20 cm².
Biochemical analyses and digital images were used to document and evaluate the inflammatory response as well as the reparative process of the surgical wound.
Patients in the group that actually received laser therapy demonstrated a reduction in wound area temperature as well as erythrocyte sedimentation rate (ESR) compared to the placebo group, showing that there was better control of inflammatory, reparative and analgesic processes.
LLLT therefore reduced biochemical markers and wound temperature, indicating a good ability to control inflammatory processes.
In addition, oedema and pain decreased after therapy and surgical wound healing improved.
A diode laser system was used to treat 17 patients with nail disorders: nine patients with chronic paronychia and eight patients with ingrown toenails (onychocryptosis).
Stage I ingrown toenails (according to Zaias N classification) or subcutaneous ingrown toenails (according to Baran R & Dawber RPR classification) were treated with LLLT.
The laser system emitted a 150 mW continuous wave beam at 830 nm in the near-infrared on a small round spot about 1 cm in diameter, delivering an incident dose of about 45 J/cm2 per spot.
The laser beam was applied to six spots on the fingers of patients with chronic paronychia and to fifteen spots on the fingers of patients with ingrown toenails for fifteen seconds per spot.
The effect was evaluated and reported by the patients themselves based on clinical findings on a scale of zero to ten.
Scores according to the results obtained
0-2 Excellent
3-5 Good
6-7 Sufficient
8-10 Poor
For paronychia, 3 subjects reported scores that were in the excellent range, 5 in the good range and one in the sufficient range. For ingrown toenail, 5 subjects reported scores in the excellent range, 2 in the good range and one in the sufficient range.
Thus, 88% of the patients were satisfied with the treatment at the end of the session cycle.
After approximately 5±4 sessions of LLLT (2 to 14 days), symptoms improved satisfactorily in most cases.
This is why, LLLT can be a valuable tool for the treatment of patients with ingrown toenails in their early stages, especially due to its non-invasiveness, absence of pain, along with the fact that it is well tolerated, and has no side effects.
Our laser therapy videos
Laser therapy and its applications:
Laser therapy makes it possible to treat a broad range of musculoskeletal and skin disorders, promoting their healing
Learn more
Laser therapy is also used in podiatry and is highly indicated in the treatment of onychomycosis, vascular ulcers, wounds and lesions.
Learn more

